Welcome to
Elite Health & Beauty Bar & Spa
Living With Lymphedema
We are here for you!
Lymphedema
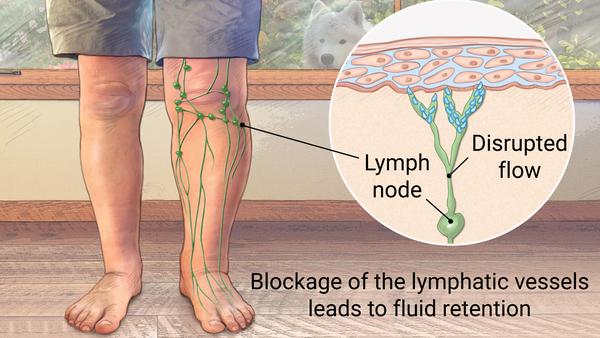
Lymphedema is a build-up of lymph fluid in the fatty tissues directly underneath the skin. This build-up may cause swelling and discomfort.
Lymphedema can develop when there is damage to the lymphatic system. The injury or damaged to lymph nodes and vessels can cause a disruption in lymphatic drainage, where lymphatic fluid doesn’t drain properly from your body, causing lymph fluid to drain into the soft tissues, which causes swelling of the affected area. This can happen anywhere in the body, the face, neck, trunk, abdomen (stomach), or genitals. but it’s most common in the arms and legs.

It’s very important to understand that lymphedema can sometimes become severe and cause significant problems and is often a long-term or chronic condition. The condition can range between mild with minor swelling and discomfort, to severe, when swelling is extensive, bringing with it secondary skin changes. If you develop lymphedema, a skin infection can be a serious problem. Therefore early, and careful management is vital to help reduce symptoms and possibly prevent the condition from getting worse.
Treatment of lymphedema includes treating swelling and prevention of infections. Exercise, compression garments, manual lymph drainage, thorough skin care, therapy and a healthy lifestyle can all help control your swelling.
Let’s visit and take a look at the lymph system
The lymph or lymphatic system is part of our body’s immune system. A system of lymph nodes, ducts or vessels, and organs that operates simultaneously to collect and carry clear lymph fluid through the body tissues to the blood stream. This system is responsible for filtering out waste products from our body’s. It filters out cellular debris and transports white blood cells to fight infection throughout the body. When you are sick, it helps filter out toxins, bacteria, and viruses.
- Lymph fluid circulates through the body and contains proteins, salts, and water. Lymph is made of proteins, fats, glucose, salts, blood cell fragments and water, as well as white blood cells, which help fight infection. The plasma protein molecules in lymph are large. Disruption to the lymphatic system can make filtering out these protein molecules harder. Lymphedema is a protein-rich swelling and bacteria feeds on protein – which means a person with lymphedema is more likely to get infections. Avoiding cuts, scrapes or any trauma to the affected region is very important.
- Lymph vessels or ducts have one-way valves that work with body muscles to help move the fluid through the body and control the flow.
- Lymph nodes are small, bean-sized glands along the lymph vessels that work to help filter foreign substances, such as tumor cells and infections. Lymph nodes are in many parts of the body, including the neck, armpit, chest, abdomen, and groin.
- The tonsils, adenoids, spleen, and thymus are also parts of the lymph system.
How Does Lymphedema Start?
Lymphedema can occur when the lymph system is damaged, which can prevent the lymph fluid from returning to the blood. For people with cancer, the build-up of lymph fluid can be caused by
Causes and risk factors for lymphedema include:
- Breast cancer surgery can increase risk of lymphedema in these ways:
- When axillary lymph nodes (under the arm) are removed, lymph vessels are damaged.
- Radiation therapy can cause increased inflammation to the skin, requiring an increased lymphatic load. Radiation damages the top layer of skin and decreased drainage is due to reduced ability of the skin to stretch.
- Chemotherapy causes fibrosis (abnormal scarring) to lymphatic vessels, resulting in impaired transport of lymph throughout the system.
- Treatment for other types of cancer: Whenever the lymph system is affected the risk goes up for lymphedema. There is more risk in treatment of prostate, pelvic area cancers, lymphoma, and melanoma; head and neck cancers often cause lymphedema in the face and neck. These areas are closer to larger numbers of lymph nodes and vessels that may be removed or damaged. A tumor may also block lymphatic drainage.
- Trauma: The lymphatic system is very close (about 1 cm, or .4 inch) to the skin’s surface. Any trauma can disrupt drainage or permanently damage lymphatic vessels or lymph nodes. Crushing injuries, burns and other traumas to the body can damage the lymph system, but even surgical incisions and scar tissue formation can act as a barrier for proper drainage.
- Vascular impairments: The venous system is responsible for re-routing 80% to 90% of the total fluid in the body. If there is a venous insufficiency or damage to the vascular system, the lymphatic system acts to help filter out fluid. But if a chronic issue with the vascular system is left untreated, the lymphatic system will eventually be unable to carry this large lymphatic load and swelling will start. An untreated chronic venous insufficiency will turn into lymphedema.
- Infection: Our bodies respond to infection with inflammation. If our system is at risk for lymphedema, an infection may cause an onset. And if the infection is severe, it can damage lymphatic vessels and nodes. (There’s a type of lymphedema caused by parasitic infection called filariasis, but isn’t common in the U.S.)
- Obesity: In addition to being overweight, adipose (fat) tissue disorders can make one more likely to have lymphedema. Excess fat can press down on superficial lymphatic vessels and nodes, decrease lymphatic drainage and cause swelling. Keeping a healthy weight is part of treatment for lymphedema.
- Cardiac impairments: This happens especially in cases of congestive heart failure. The lymphatic ducts empty lymph back into the heart. If there is decreased heart function, people may notice swelling to their legs and weight gain. If not treated properly, damage can occur to the lymphatics as well as to the skin, causing lymphedema.
- Kidney Disease: Your kidneys work to remove extra fluid and waste products from your body. If there is impaired kidney function this can cause decreased ability of the body to remove fluid. This can back up to the entire system, causing swelling that may lead to lymphedema.
It’s important to know the signs and symptoms of lymphedema, so it can be recognized and treated right away.
Common signs and symptoms of lymphedema can include:
- Swelling in part of the body (such as your breast, chest, shoulder, arm, or leg)
- Noticeable thickening of the skin, tightness or hardness, changes in texture, skin redness, or feeling hot
- New aching, tingling, numbness, burning or itching sensation or other discomfort in the area. Uncomfortable heaviness or fullness.
- Less movement or flexibility in joints.
- Trouble fitting your clothes, rings, watches, and/or bracelets feeling tight even though you haven’t gained weight.
- Difficult to see or feel veins and tendons in your hands and feet.
- Your arm or leg appears to be of slightly different size.
- Puffiness of the skin.
- If lymphedema develops after breast cancer treatment it can affect the breast, chest, and underarm, as well as the arm closest to the surgery.
- After cancer in the abdomen or pelvis has been treated, lymphedema may appear as swelling of the abdomen, genitals, or one or both legs.
- Treatment of tumors in the head and neck area might lead to lymphedema in the face and neck.

The severity of lymphedema is often described by its stage:
Stage 0: No swelling, but subtle symptoms such as feeling the affected area is heavy or full, or that the skin is tight.
Stage 1: Swelling of the affected area. There is increased size or stiffness of the arm or leg or affected area. For the arms or legs, the swelling improves when the arm or leg is raised.
Stage 2: More swelling than stage 1, which does not improve when the arm or leg is elevated. The affected area is hard and larger in size than stage 1.
Stage 3: Much more swelling than stage 2. The swelling might be so severe that you cannot lift or move the arm or leg on your own without using your other arm. The skin can become very dry and thick. The swelling can cause fluid to leak from the skin or blisters to form.
There is more risk for infection in the affected area that is at the later stages, such as stage 2 or 3. The early stages (stages 0 and 1) of lymphedema are often reversible, while the later stages (stages 2 and 3) tend not to respond as well to treatment. Therefore, it’s very important to see your health care provider as soon as you notice any concerning symptoms.
There are two types of lymphedemas
Primary lymphedema comes from rare, inherited conditions when the lymphatic system doesn’t develop properly. Lymphedema from these conditions can appear at these ages:
- Infancy: Called Milroy’s disease (congenital lymphedema).
- Puberty, during pregnancy, or up until age 35: Called Meige’s disease (lymphedema praecox).
- After age 35: A rare, late-onset lymphedema (lymphedema tarda) can cause lymphedema after 35. This type usually causes swelling only in the legs.
Secondary lymphedema is the most common form of lymphedema. It is caused by disruption to the drainage of the lymphatic system that occurs with trauma. In the U.S., cancer treatments are the most common cause of damage to the lymphatic system. However, not everyone who has cancer treatment develops lymphedema.
Cellulitis is an infection in the tissues just under your skin. It can lead to lymphedema. Cellulitis is an urgent medical problem that you need to tell your doctor about right away. Signs and symptoms of cellulitis include redness, warmth, pain, and possibly cracking or peeling of the skin in the area that’s infected. Fever and flu-like symptoms may also be present. If it becomes a repeated problem, antibiotics may be needed to keep it under control. Lymphedema can also lead to cellulitis, so it is important to watch for signs and symptoms.
Lymphedema Bandaging
Compression garments help to stop lymphoedema getting worse. They can reduce mild swelling. Your specialist will usually recommend multi-layered bandaging first if you have severe lymphoedema. The garments vary in how much pressure they put on the tissues. If numbness, tingling, increased pain, coolness, and/or swelling occurs, the wrap is too tight. Re-wrap the area every 3-4 hours or at least once per day because the bandage will loosen. Do NOT sleep with the bandage on. Elevation helps slow and reduce swelling at night. Re-wrap the following morning.
Contraindications for CDT
Complete Decongestive Therapy (CDT) involves manual lymph drainage (MLD) & compression bandaging (as well as skin care & exercise). In some instances, CDT should not be performed. These occasions include:
- Active Infection caused by pathogens. During localized infection, lymphatic vessels constrict to prevent pathogens & other harmful matter from escaping the area & entering the rest of the circulation. When MLD is performed, the spasm may be counteracted. This would allow normal flow to resume & potentially spread the toxin(s). In general, a person needs to be on an antibiotic for 2-3 days with signs of improvement (no fever; swelling, redness, pain have subsided) before MLD may resume. Some professionals wait up to 7-10 days before resumption as the inflammatory response can last that long. The multi-layer compression bandaging may hinder the body’s inflammatory response.
- Deep Vein Thrombosis / Thrombophlebitis. MLD stretches the skin & may potentially dislodge a blood clot. Mild compression can be beneficial as it encourages clot adhesion to the vascular wall. It is recommended to have physician approval prior to application.
- Cardiac Edema. All lymph fluid returns to the circulatory system at the venous angles. In acute congestive heart failure, the heart is already overwhelmed by the volume of fluid being managed. MLD only increased the load the heart must manage. The same is true for bandaging. Additionally, in acute cases of heart failure, the cause of swelling is the failing of the heart, so CDT will not help.
- Peripheral Artery Disease. While MLD is not a concern, bandaging can compromise an already reduced arterial blood flow. Arterial pressure in the foot below 70 mmHg (as measured by Doppler Ultrasound) is a contraindication for compression.
- Active Cancer. Malignant tumors with a tendency to metastasize are an absolute contraindication for MLD as MLD only speeds up lymphatic flow & cancer travels via the lymphatic system or the cardiovascular system. However, if a person is responding to chemo & the physician approves MLD, the massage may be performed (avoiding the immediate area of the tumor). In other types of cancers, MLD may be permissible with physician approval. Compression can be useful in helping to manage swelling.
There may be other occasions when aspects of CDT is not appropriate.